FILARIASIS
Filariasis is caused by several round, coiled and thread-like parasitic worms belonging to the family filarioidea. Wuchereria bancrofti, Brugia malayi and Brugia timori are the parasites after getting deposited on skin penetrate on their own or through the opening created by mosquito bites and reach the lymphatic system and eventually cause lymphatic filariasis.
Lymphatic Filariasis (LF), commonly known as elephantiasis is a disfiguring and disabling disease, usually acquired in childhood. In the early stages, there are either no symptoms or non-specific symptoms. Although there are no outward symptoms, the lymphatic system is damaged. This stage can last for several years. Infected persons sustain the transmission of the disease. The long term physical consequences are painful swollen limbs (lymphoedema or elephantiasis). Hydrocele in males is also common in endemic areas.
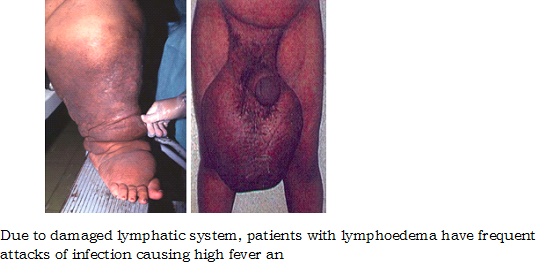
Due to damaged lymphatic system, patients with lymphoedema have frequent attacks of infection causing high fever and severe pain. Patients may be bed-ridden for several days and normal routine activities become difficult. Such attacks not only cause acute physical suffering but also directly impede the earning capacity of the individual.
Lymphatic filariasis is estimated to be one of the leading causes of disability worldwide. Elimination of the disease is an important tool for poverty alleviation and economic development.
There are two types of lymphatic filariasis in India.
1. Brugian filariasis: Lymphadenitis (swollen and painful lymph node) occurs episodically, most commonly affecting one inguinal lymph node at a time. Characteristically, elephantiasis involves the leg below the knee but occasionally it affects the arm below the elbow. Genital lesions or chyluria (milky colour urine) do not occur in brugian filariasis. This is not reported in Tamil Nadu.
2. Bancroftian filariasis: The lymphatic vessels of the male genitalia are most commonly affected in bancroftian filariasis, producing episodic funiculitis (inflammation of the spermatic cord), epididymitis and orchitis. Adenolymphangitis of the extremities is less common. Hydrocele is the most common sign of chronic bancroftian filariasis, followed by lymphoedema, elephantiasis and chyluria. The swelling involves the whole leg, the whole arm, the scrotum, the vulva or the breast. The fluid of hydrocele and chyluric patients may contain microfilariae, even when they are absent from the blood. Chyluria occurs intermittently and is more pronounced after a heavy meal. It is often symptomless, but some patients complain of fatigue and weight loss, resulting from loss of fat and protein.
Magnitude of disease
Filariasis has been a major public health problem in India next only to malaria. The disease was recorded in India as early as 6th century B.C. by the famous Indian physician, Susruta in his book Susruta Samhita. In 1709, Clarke called elephantoid legs in Cochin as Malabar legs.
The discovery of microfilariae (mf) in the peripheral blood was made first by Lewis in 1872 in Calcutta (Kolkata).
Transmission of Lymphatic Filariasis
Lymphatic filariasis is transmitted through the bite of infected Culex quinquefasciatus mosquito in Tamil Nadu. Brugia malayi is transmitted by Mansonia annulifera, M.uniformis and M. Indiana in Kerala.
Culex quinquefasciatus breeds in association with human habitations and is the domestic pest mosquitoes, preferring polluted waters, such as sewage and sullage water collections including cesspools, cesspits, drains and septic tanks. In the absence of such type of water collections, they can breed in comparatively clean water collections also.
Adult Filarial worm
In the adult stage, filarial worms live in the vessels of the lymphatic system. Lymphatic system is the network of lymph nodes and lymph vessels that maintains the fluid balance between the tissues and the blood which is an essential element of the body's immune defense system.
The adult produces millions of very small immature larvae known as microfilariae, which circulate in the peripheral blood with marked nocturnal periodicity. The worms usually live and produce microfilariae for 5-8 years.
Adult Filaria Worms inhabiting lymphatic system of man

|
The persons having circulating microfilariae are outwardly healthy but transmit the infection to others through mosquitoes. The persons with chronic filarial swellings suffer severely from the disease but no longer transmit the infection. |
In India, 99.4% of the cases are caused by the species - Wuchereria bancrofti whereas Brugia malayi is responsible for 0.6% of the problem.
Life Cycle of Filarial Parasite
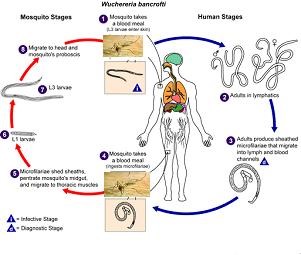
Man is the definitive host i.e. where the mature adult male and female parasites mate and produce microfilariae whereas the mosquito is the intermediate host. The adult parasites are usually found in the lymphatic system of man. They give birth to as many as 50,000 microfilariae per day, which find their way into blood circulation. The life span of microfilaria is not exactly known which preferably may survive up to a couple of months.
The parasite cycle in the mosquito begins when the microfilariae are picked up by the vector mosquitoes during their feeding on the infected person (microfilaria carrier). The microfilaria in mosquito develops into three stages and under optimum conditions of temperature and humidity; the duration of the cycle in the mosquito (extensive incubation period) is about 10-14 days. When the infective mosquito feeds on other human host, the infective larvae are deposited at the site of mosquito bite from where the infective larvae get into lymphatic system. In the human host, the infective larvae develop into adult male and female worms. The adult worms survive for about 5-8 years or sometimes as long as 15 years or more.

National Filaria Control Programme
The National Filaria Control Programme is being implemented in Tamilnadu since 1957. Indigenous cases have been reported from about 20 districts in the state. The filaria disease control activities are carried out in 43 urban areas. In these urban areas 25 control Units, 44 Night Clinics are functioning. As a unique feature 42 Filaria and Malaria Clinics are functioning at taluk level in 5 districts . The Diethyl Carbamazine citrate (DEC) tablets is given to the Lymphatic Filaria cases as per GoI norms besides morbidity management of LF cases.
Strategy for Elimination of Lymphatic Filariasis
Mass Drug Administration programme with DEC tablet was started in 1996 in Cuddalore District as a pilot project. Later DEC and Albendazole tablets were given to the eligible population inall the Filaria endemic Districts, namely Kancheepuram, Thiruvallur,Vellore, Tiruvannamalai Cuddalore, Villupuram, Trichy, Perambalur,Ariyalur, Pudukottai, Thanjavur,Thiruvarur,Nagapattinam, Nagarcoil and certain areas of Karur, Krishnagiri, Virudhunagar, Thirunelveli, Thoothukudi,Madurai and certain wards in Chennai Corporation .
Self care practices training on Foot hygiene for the Lymphoedema cases is imparted by the public Health staff.
Hydrocelectomy is done in District Hospital, Medical College Hospital, Block Primary Health Centers etc.
Validation through Transmission Assessment Survey (TAS)
As per WHO guidelines, Transmission Assessment Survey (TAS) had been completed in all the 20 Filaria endemic districts in Tamilnadu and qualified for MDA stoppage.
Lymphoedema Management
Filaria patients with damaged lymphatic vessels often have more bacteria on the skin than usual. The large number of bacteria on the skin, multiple skin lesions, slow lymph fluid movement and the reduced ability of the lymph nodes to filter the bacteria cause inflammation characteristic of an acute attack.
Repeated bacterial infections precipitate frequent acute attacks, which further damage the tiny lymphatic vessels in the skin, reducing their ability to drain fluid. This vicious cycle continues, aggravating the condition of the patient.
The lymphoedema management involves the following components:

Special Scheme for LF Patients
Tamilnadu Government is providing financial assistance of Rs.1000/- per month to the Grade IV Filaria patients.
|
| Home | Malaria | Dengue | Chikungunya Fever | Japanese Encephalitis | Filaria | Leprosy | Notifiable Diseases| Epidemic G.O. | |